UCLA scientists find cancer immunotherapy drug may be useful against HIV
EghtesadOnline: In lab experiments, immune T cells re-engineered to target receptors on HIV successfully killed several strains of the virus.
Researchers at UCLA found in lab experiments that reprogramming T cells to recognize HIV allows them to kill the virus rather than being invaded.
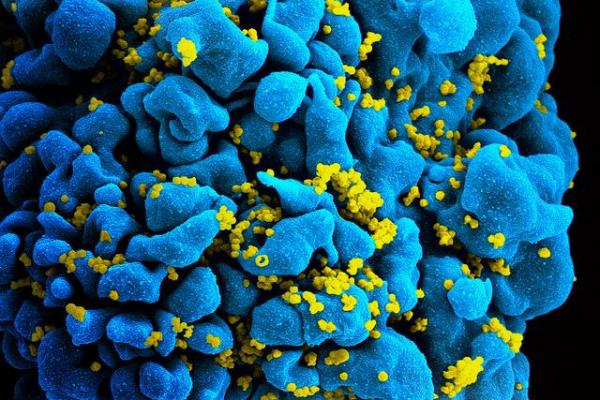
According to ISNA, HIV weakens the immune system by replicating quickly and infecting immune T cells, pictured.
A method of reprogramming immune cells to attack cancer may also work to help the body effectively fight off HIV, according to early research.
Researchers at the University of California Los Angeles found reprogramming immune T cells using recently discovered antibodies allowed them to attack and kill HIV in lab experiments, suggesting the method can be applied to diseases beyond cancer.
Immunotherapy is based on creating chimeric antigen receptors, or CARs, which are designed to seek and kill specific cells with virus or tumor proteins.
Increasingly, reprogramming these cells to attack cancer is proving effective. UCLA researchers decided to revisit the concept for battling HIV because while experiments to do so did not work in the past, antibodies discovered in the last few years can target more virus strains.
These "broadly neutralizing antibodies" were thought to potentially be able to outlast HIV, which overtakes the immune system by hiding in different T cells and replicating too quickly for the body's defenses to respond.
For the study, published in the Journal of Virology, researchers re-engineered seven of the antibodies as artificial CAR-T cell receptors, finding they all had varying degrees of success killing HIV in the lab.
The method shows promise, researchers said, and they plan to move forward figuring out how to get the CAR-T cell receptors into humans for testing. Dr. Otto Yang, a professor of medicine at UCLA and lead researcher on the study, expressed caution before those tests begin.
"What works in a test tube doesn't necessarily work in a person," Yang said in a press release.


